Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
How to Care for Your Child's Feet
It is never normal for a child to experience pain in his or her feet. Foot pain that lasts more than a few days and limits a child’s ability to walk should be examined by a podiatrist. Many adult foot ailments originate in childhood and may be present at birth. Common foot issues that are experienced by children are pediatric flat foot, Sever’s disease, ingrown toenails, and plantar warts.
A child’s foot grows rapidly during the first year, allowing it to reach almost half of their adult foot size. Consequently, foot specialists consider the first year to be the most crucial point in the foot development process. There are ways you can help ensure that your child’s foot develops properly. One way is to carefully look at your baby’s feet. If you notice any deformities, you should immediately seek professional care. You should also loosely cover your child’s foot, since tight coverings may prevent movement and inhibit normal development. Another tip is to change the baby’s positioning throughout the day. If your baby lies down in one spot for too long, it may put an excess amount of strain on the feet and legs.
It is best that you try not to force a child to start walking. Children will begin to walk when they are both physically and emotionally capable to do so. You should also avoid comparing your child’s walking progress with other children because the age range for independent walking may range. When your child’s feet begin to develop, you may need to change both their shoe and sock size every few months to allow room for their feet to grow.
Kids are sometimes prone to splinters, cuts, and severe injuries because they tend to walk around barefoot. This also makes them more susceptible to developing plantar warts which is a condition caused by a virus that invades the sole of the foot through breaks in the skin. These ailments can be avoided by making sure your child wears shoes in unsanitary environments. You should also wash any minor cuts or scrapes on your child’s feet. It is a myth that exposure to fresh air will heal injuries; fresh air will only expose your child’s cuts to germs.
As a parent, you should ensure that your child’s feet are developing properly and are being properly maintained. Consequently, it is important that you perform routine inspections on his or her feet to detect any injuries or deformities in their early stages. Early detection and treatment will help to ensure that your child does not develop any serious foot conditions.
Causes and Symptoms of Flat Feet
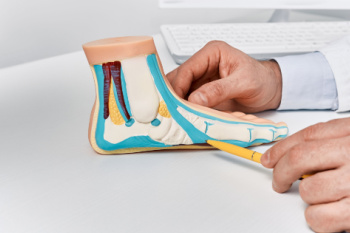
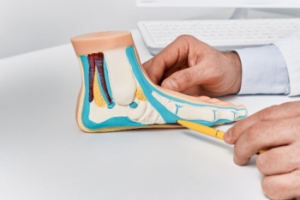
Flat feet, or fallen arches, occur when the arches of the feet do not develop properly or collapse over time. This condition can be caused by genetic factors, injury, arthritis, or the natural aging process. Obesity and pregnancy may also contribute to the development of flat feet due to increased pressure on the arches. Common symptoms include foot pain, particularly in the heel or arch area, swelling along the inside of the ankle, and difficulty standing on tiptoe. Flat feet can lead to problems with walking or running and may cause discomfort in the legs and lower back. Proper diagnosis and treatment by a podiatrist can help to manage symptoms and prevent further complications. If you have flat feet, it is suggested that you are under the care of this type of doctor who can help you manage this condition and guide you toward relief solutions.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from New York, NY. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
Athlete’s Foot Relief and Prevention Tips
 Athlete's foot, or tinea pedis, is a common fungal infection affecting the skin of the feet, typically occurring between the toes. There are three main types of athlete’s foot, which are interdigital, moccasin, and vesicular. Interdigital athlete's foot typically occurs between the toes and is characterized by itching, scaling, and sometimes maceration of the skin. Moccasin athlete's foot affects the soles and sides of the feet, presenting as dry, thickened, and scaly skin that can sometimes crack. Vesicular athlete's foot features fluid-filled blisters, often appearing on the instep, and can cause intense itching and discomfort. The infection is caused by dermatophytes, which are fungi that thrive in warm, moist environments like locker rooms, public showers, and swimming pools. Risk factors include wearing tight, non-breathable footwear, sweating heavily, and walking barefoot in damp communal areas. Symptoms include itching, burning, peeling, and cracked skin, often accompanied by redness and blisters. Athlete's foot is extremely contagious and can spread through direct contact with infected skin or contaminated surfaces. Treatment involves antifungal medications, available as creams, sprays, or oral prescriptions, depending on the severity. If you have athlete’s foot, it is strongly suggested that you visit a podiatrist who can effectively treat the infection, which often includes prescribed medication.
Athlete's foot, or tinea pedis, is a common fungal infection affecting the skin of the feet, typically occurring between the toes. There are three main types of athlete’s foot, which are interdigital, moccasin, and vesicular. Interdigital athlete's foot typically occurs between the toes and is characterized by itching, scaling, and sometimes maceration of the skin. Moccasin athlete's foot affects the soles and sides of the feet, presenting as dry, thickened, and scaly skin that can sometimes crack. Vesicular athlete's foot features fluid-filled blisters, often appearing on the instep, and can cause intense itching and discomfort. The infection is caused by dermatophytes, which are fungi that thrive in warm, moist environments like locker rooms, public showers, and swimming pools. Risk factors include wearing tight, non-breathable footwear, sweating heavily, and walking barefoot in damp communal areas. Symptoms include itching, burning, peeling, and cracked skin, often accompanied by redness and blisters. Athlete's foot is extremely contagious and can spread through direct contact with infected skin or contaminated surfaces. Treatment involves antifungal medications, available as creams, sprays, or oral prescriptions, depending on the severity. If you have athlete’s foot, it is strongly suggested that you visit a podiatrist who can effectively treat the infection, which often includes prescribed medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from New York, NY. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Characteristics of Hammertoe

Hammertoe is a foot deformity characterized by an abnormal bending of the toe joints, causing the affected toes to resemble a hammer or claw. This condition typically affects the second, third, or fourth toes, although it can occur in any toe. Hammertoe often develops gradually over time, due to factors like ill-fitting shoes, foot structure abnormalities, or muscle imbalances. One of the noticeable features of hammertoe is the bending of the toe joints, resulting in a permanent, abnormal position that may cause pain, discomfort, or difficulty walking or wearing shoes. Other characteristic symptoms include corns or calluses forming on the tops of the affected toes due to friction and pressure from rubbing against footwear. Additionally, individuals with hammertoe may experience limited range of motion in the affected toes, making it challenging to straighten or flex them fully. If you notice a deformity in your toes, it is suggested that you make an appointment with a podiatrist for an exam, a diagnosis and the appropriate treatment.
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists of New York, NY. Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.