Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
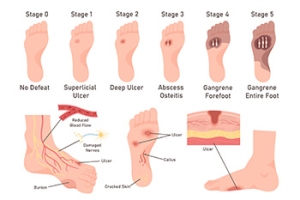
Managing Diabetic Foot Ulcers
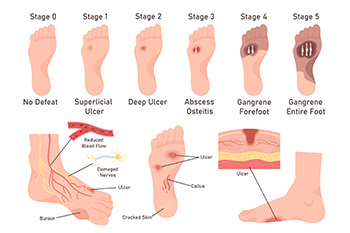
Diabetic foot ulcers are open sores or wounds that commonly occur on the bottom of the foot in people with diabetes. They are caused by poor circulation, nerve damage or neuropathy, high blood sugar levels, and repetitive pressure or trauma to the feet. Because nerve damage can dull pain sensations, many patients may not feel the ulcer forming until it becomes severe. Symptoms include redness, swelling, drainage, or a foul odor. The area may feel warm, and in some cases, there can be pain, although many feel little to none due to neuropathy. Untreated ulcers can lead to serious infections or even loss of limb. A podiatrist plays a key role in managing diabetic foot ulcers by offering treatments like offloading that reduce the pressure on the wound, wound debridement to remove dead tissue, specialized dressings, and infection control. Custom orthotics or diabetic shoes may also be recommended. If you have diabetes and have a foot ulcer, it is suggested that you are under the care of a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from New York, NY. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Managing Heel Pad Syndrome

Heel pad syndrome, also known as fat pad atrophy, occurs when the thick layer of fatty tissue beneath the heel thins out, reducing its ability to absorb shock. This can lead to deep, aching heel pain that worsens with prolonged standing or walking. Common causes of heel pad syndrome include age-related degeneration, obesity, repetitive impact activities, wearing improper footwear, and prior heel injuries. People who walk barefoot on hard surfaces may place additional stress on the heel, increasing the risk of pain. A podiatrist can evaluate heel pad function and recommend appropriate treatment to relieve pressure on the heel. Supportive orthotics and well-cushioned footwear can help reduce discomfort during daily activities. In addition, specific exercises, such as calf stretches, heel raises, and ankle range-of-motion movements, are often used to improve foot control and reduce stress on the heel. If you are suffering from heel pain, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and proper treatment.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of New York, NY. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions, please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
What Causes Thick Toenails?

Thick toenails can result from several causes, including toenail fungus, aging, or past trauma to the nail. Fungal infections are one of the most frequent culprits, causing the nail to become discolored, brittle, and misshapen. As people age, nail growth slows and thickens naturally. Injuries, even minor ones, can also damage the nail bed, leading to long-term thickening. Thick toenails may appear yellow, white, or brown, and often feel hard, rough, or crumbly. They can be painful, especially when wearing shoes. Trimming them often becomes difficult. A podiatrist can determine the exact cause through examination or lab testing. Treatment depends on the cause and includes topical or oral antifungal medications, trimming and thinning the nail, or permanent nail removal, in severe cases. Proper foot hygiene and footwear advice are also part of long-term care. If you have toenail fungus, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment solutions.
For more information about treatment, contact one of our podiatrists of New York, NY. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Foot Arch Stretches Can Help With Plantar Fasciitis

Foot arch stretches can play an important role in both curing and preventing plantar fasciitis by improving strength, flexibility, and circulation in the foot. Regularly performing a step stretch helps elongate the plantar fascia and Achilles tendon, reducing heel pain. Calf raises strengthen the muscles that support the arch and ankle. Doming exercises improve control of the intrinsic foot muscles, which stabilize the arch. The toe spread and squeeze technique activates small foot muscles that are often neglected but essential for maintaining proper alignment. Additionally, towel curls engage the arch by encouraging gripping and curling motions that build strength. If you suffer from arch pain as a result of plantar fasciitis or other reasons, it is suggested that you consult a podiatrist who can offer you effective treatment and relief tips.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact one of our podiatrists from New York, NY. Our doctors can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctors to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions, please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Exercise for Your Feet
Foot and ankle pain can be a nuisance in a person’s life, especially if it happens frequently. The best way to prevent this type of pain, is to exercise often. Regular exercise of the foot includes stretching and strength exercises. Stretching exercises can help prevent injuries such as a sprained ankle, while strength exercises can prevent ailments such as plantar fasciitis.
Stretching exercises can help improve flexibility and the foot and ankle’s range of motion. These exercises can certainly help with those who participate in high-energy activities such as sports. Many athletes routinely perform foot and ankle exercises to prevent injuries like sprained ankles, which are common injuries where the tendons in the ankle are over stretched. Strength exercises help develop foot muscles for better support and protection.
Most exercises are simple and can be done at home, either standing or sitting. One chair exercise is called “limber up”. In this exercise, a person would start by sitting down with their feet flat on the floor. Then lift one leg up so the feet are not touching the floor, then rotate your foot clockwise 15-20 times, and 15-20 times counterclockwise. Repeat the same process with the opposite leg. Another sitting exercise helps stretch the back of your heel and requires an exercise band. It begins by looping the band around a heavy piece of furniture, or something stable that will not be moved when the band is tugged or pulled. Then sit directly in front of it, and slide one foot into the loop, so that the band curves around the forefoot. Start by pulling the forefoot back and holding it for 5-10 seconds. Doing this 10-15 times on each foot, will stretch the back of your heel, increasing your flexibility.
Foot exercises that require standing are also just as easy and simple. Referred as the “Achilles Stretch”, this exercise stretches the Achilles tendon, making it more flexible, helping prevent foot, ankle, and leg pain. It begins by first standing and facing the wall, with the arms outstretched and the palms on the wall. Then place one foot behind another keeping the back leg straight, and the forward leg bending at the knee. Make sure both heels are flat on the floor and adjust your stance accordingly. With your hips, lean forward to feel the stretch, you can also adjust the distance from your feet to feel the stretch in various parts of the calf. Make sure to hold the stretch for about 30 seconds and repeat the same process 3 times with each leg. An even easier foot exercise is simply walking on sand. Walking barefoot on sand both strengthens and stretches your feet.
Doing these exercises regularly can help prevent many foot and ankle problems. Other foot exercises can even relieve pain. For example, those affected with plantar fasciitis can simply sit down on a chair, and then place a tennis ball below their affected foot. By rolling the ball under the foot, and increasing or decreasing pressure, pain will be relieved. With any exercise, it is always important to do a small warmup such as walking a few laps around the house to get the blood flowing. If after doing an exercise to relieve pain such as the tennis ball exercise, or are unsure that your execution is correct, be sure to contact a podiatrist for further instruction.